Climbing Everest and Its Effect on Everything
Insights from the Myofocus Education Seminar
Having had the privilege of spending 4 days helping teach a seminar with the Myofocus Education team, I wanted to bring some attention to some concepts fresh in my mind in this month’s blog. It's built around a few different points and I hope it will make you think about maternal, child, and adult airway health and the brain.
Oral Myotherapy and Tongue Tie
The seminar was teaching about oral myotherapy and tongue tie, allowing me to talk about my favorite areas, including mouth breathing and the developmental impacts of primitive reflexes upon craniofacial development and long-term health outcomes. The final guest lecturer for the course on day four was the fabulous Dr. Jeevanan Jahendran, an ear nose throat specialist, and out-of-the-box thinker, and an all-around great human.
Mouth Breathing and Primitive Reflexes
Primitive reflexes play a crucial role in the early stages of development. These reflexes, such as the Moro reflex, ATNR (Asymmetric Tonic Neck Reflex), and TLR (Tonic Labyrinthine Reflex), are essential for survival and initial stages of development. However, if these reflexes persist beyond the typical age of integration, they can impact craniofacial development and lead to long-term health issues. For example, mouth breathing can alter the growth patterns of the face, leading to conditions such as long face syndrome, dental malocclusion, and other airway-related problems. Addressing these reflexes through therapies like oral myotherapy can have significant benefits on overall health and development.
Dr. Jeevanan Jahendran’s Lecture on the Aerodigestive Tract
Dr. Jahendran’s lecture on the aerodigestive tract was particularly insightful. He discussed the intricate relationship between the respiratory and digestive systems, highlighting how issues in one can affect the other. Key takeaways from his lecture included the importance of proper breathing techniques and the impact of respiratory health on digestion and overall well-being. His out-of-the-box thinking encouraged us to look at these systems holistically rather than in isolation.
The Impact of Oxygen Supply During Pregnancy
While I enjoyed Dr. Jahendran’s latest discussion on the aerodigestive tract, the part that got me excited was being exposed to a paper on the oxygen supply to the baby during pregnancy. The paper, called "Mount Everest in Utero" by Nicholson J. Eastman MD from 1954, is phenomenal but until now I think largely consigned to the memory hole. We have forgotten many of the important messages about human physiology that were being studied in the mid-20th century, and in some cases, your degrees may never have taught this to you as mine did not.
Understanding Fetal Hypoxia
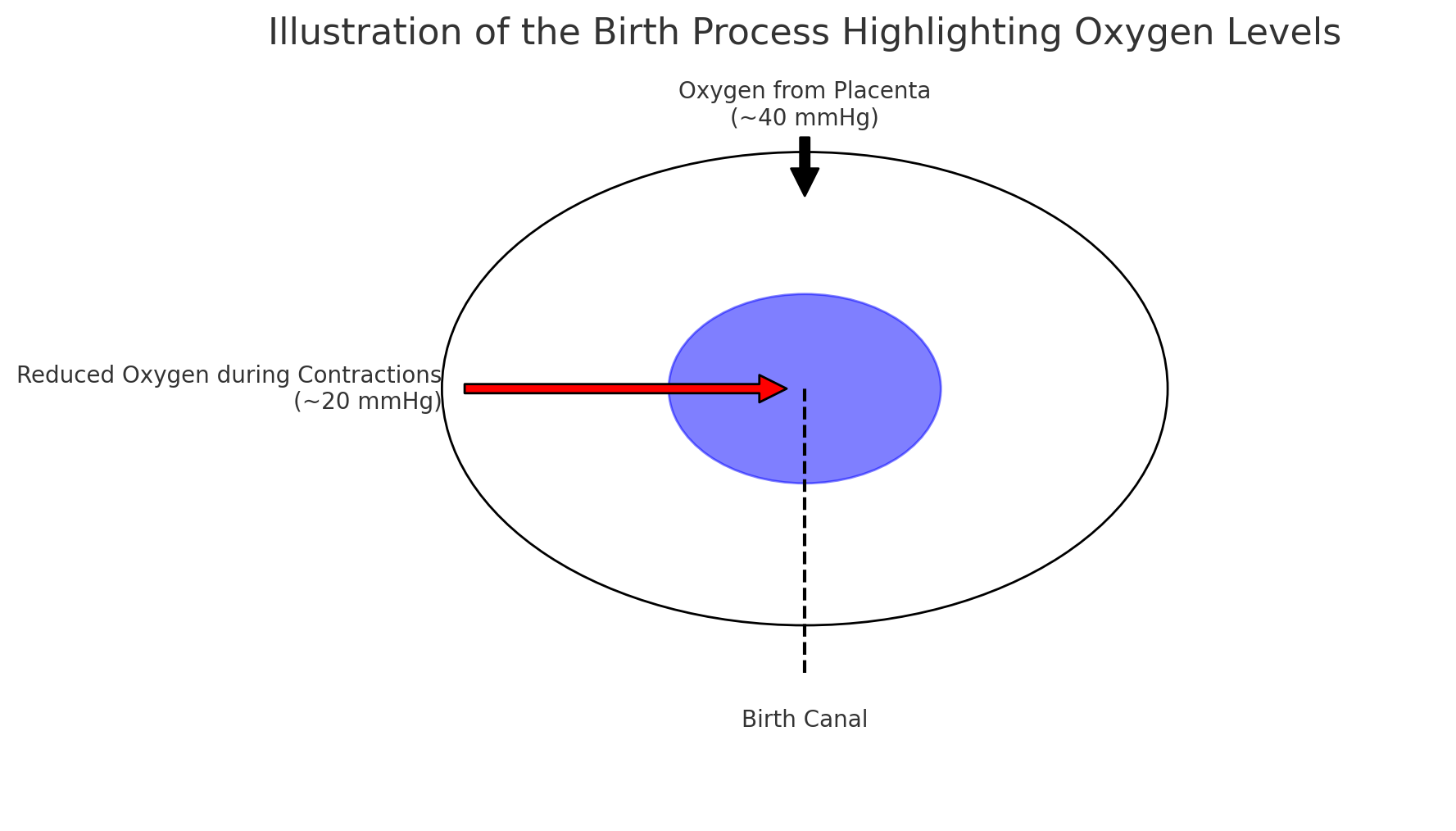
During the birth process itself, the fetus is subjected to a tremendous degree of hypoxia but comes out fine in the majority of cases. The extreme hypoxic insult during the process of birth has led perinatal physiologists to call the process of birth the “Valley of Shadow of Birth.”
Hypoxia from a sudden drop in oxygen with trauma or poor breathing and hyperoxia (high oxygen especially in relation to the low oxygen environment the baby has just come from) after birth cause oxidative stress and free radical derived conditions, with oxidative stress biomarkers correlating with clinical outcomes for the child.
Birth and the “Valley of Shadow of Birth”
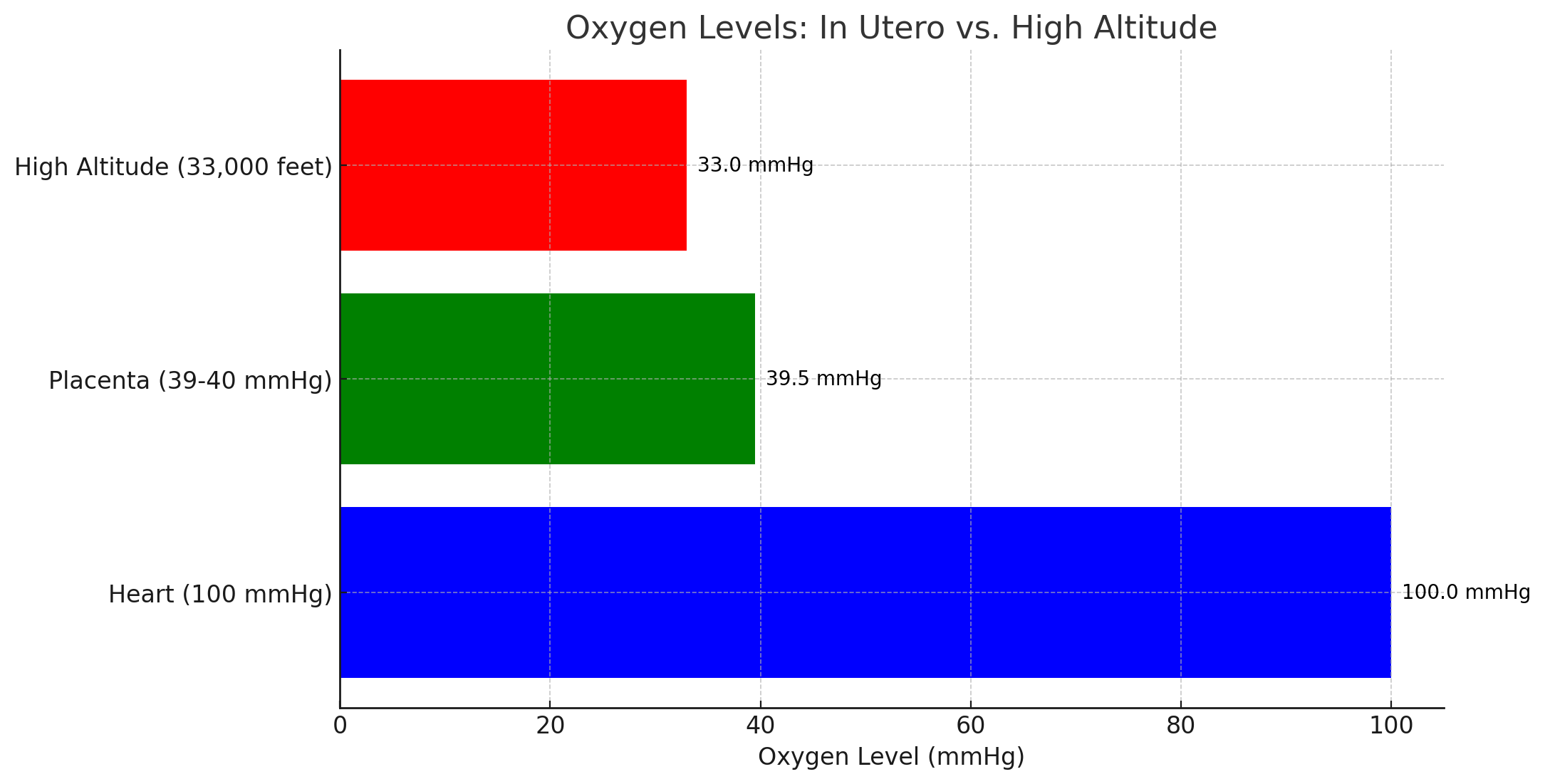
To get to the point, the environment that the baby is growing in has profound outcomes on individual health as well as on the health of our society. As it turns out, there is a significant difference in the partial pressure of oxygen being delivered across the placenta compared to the pressure leaving the heart at 100 mmHg. The 39-40 mmHg in the cord is equivalent to the pressure at 33,000 feet. Think of this as about a ¼ mile higher than the tip of Mt. Everest. This is a point at which humans die without oxygen.
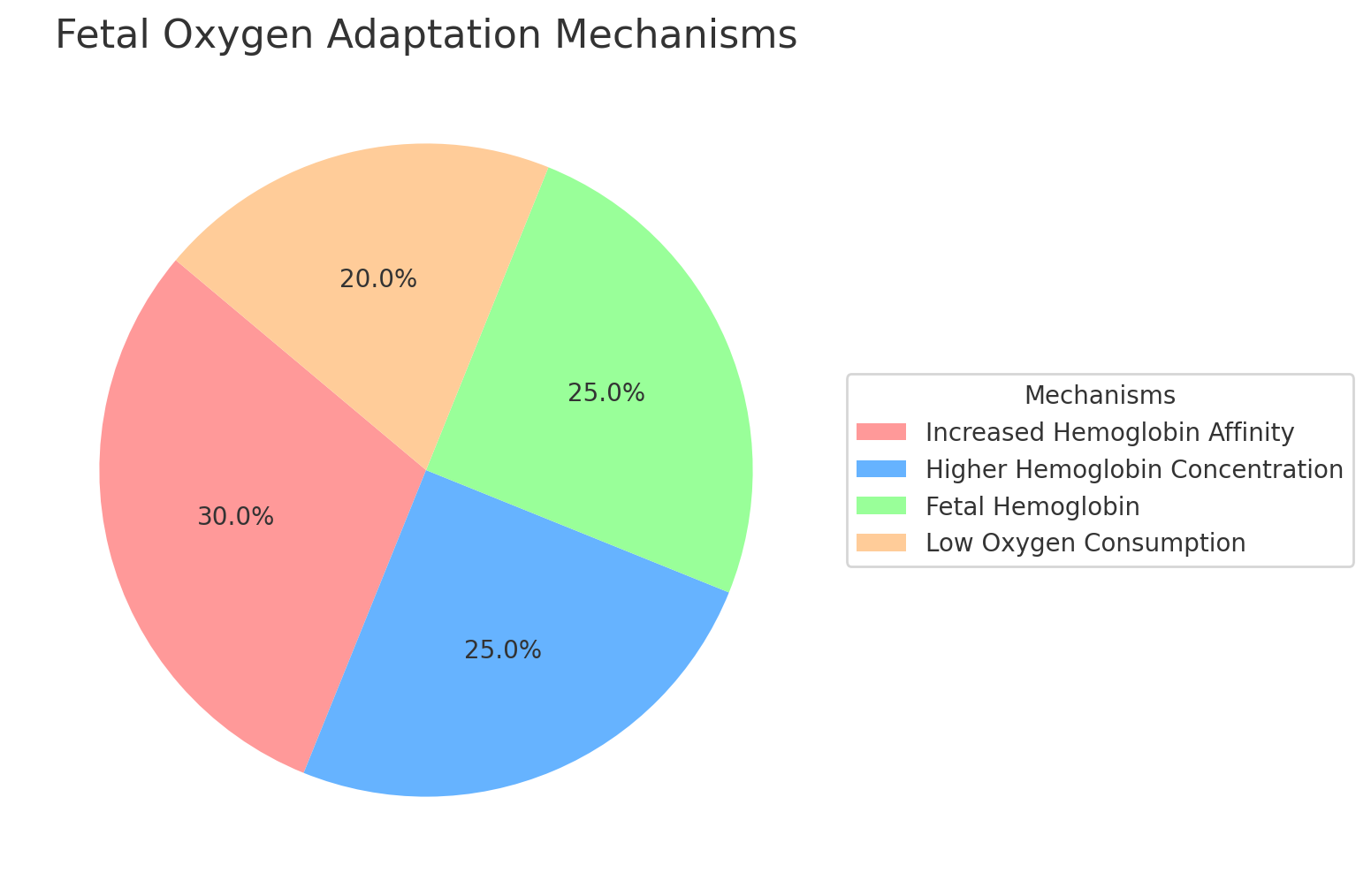
This raises all sorts of questions about how the fetus survives the truly hypoxic environment. With the fetus being unable to increase the delivery of oxygen to itself, it must manipulate the consumption level at the tissue. Another paper agreed that “it’s true that the fetal arterial PO2 levels are close to those at Mount Everest, the fetus is, however, well oxygenated for its needs.”
Maternal Stress and Its Effects on Fetal Development
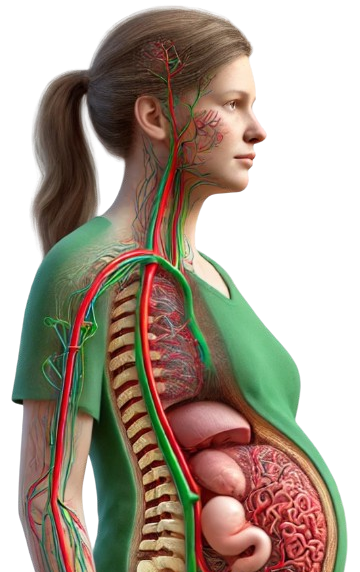
Let’s roll back a little further and consider the maternal system in relationship to the fetus’s blood supply and primitive reflexes early on in the pregnancy, say at about 5 weeks. If the mom’s system is threatened, then a survival reflex called the fear paralysis reflex will activate, driving the blood away from the uterine region to the mom’s body.
This will further lower the oxygen supply to the developing fetus, if only temporarily. This is all fine if it occurs once in a while, but imagine the effects of a high-stress environment or perhaps smoking. Adrenaline excess can either inhibit fibroblast growth or induce the differentiation of myofibroblasts that elicit strong contracture, which could significantly affect tongue and oral fascial restriction.
Cortisol and WNT Signaling in Facial Development
Under chronic stress, cortisol excess inhibits the WNT signaling genetic pathway, which I spoke about in my book "First Principles." This is fundamental for bone and facial connective tissue development and increases FGF23 production. Cortisol excess induces high inflammation and type-3 immunity. Hypoxia could be considered chronic stress for the fetus, which is shown to affect folate metabolism, creating or exposing defects in DHFR and MTHFR function. In an experiment on a rat model of folate and B12 deficient moms, neonatal hypoxia increases homocysteinemia mainly by decreasing homocysteine trans-sulfuration in developing rats under a methyl-deficient regimen. It could, therefore, potentiate the well-known adverse effects of hyper-homocysteinemia.
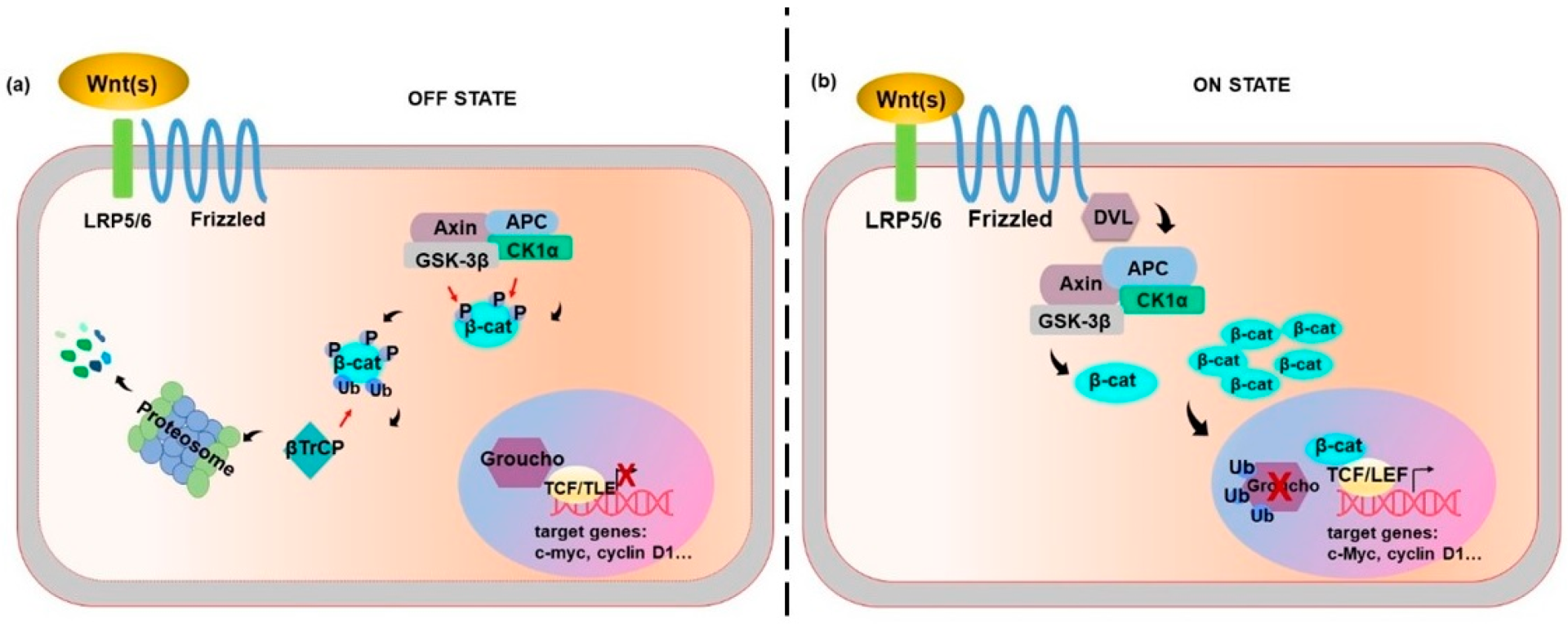
Defects in folate metabolism during facial development at that 5-12 week mark result in a significant loss of cells expressing the genes (including WNTs, and FGFs {fibroblast growth factor gene}) which are essential for facial structure formation, profoundly affecting the shape and size of the face of the developing fetus, leading to maldevelopment of the face in the child after birth and ongoing consequences in life. Thus, hypoxia can create alterations to facial growth, fascia fibroblast function, as well as altering MTHFR/DHFR metabolism in the growing child, all of which contributes to the creation of tongue fascial restriction, and maldevelopment of the cartilaginous structure of the face.
The Role of Birth Methods in Neonatal Health
The next points I want to raise for thinking are not to be taken as judgment but to raise questions as to the direction our society is going. As I spoke about in "First Principles," from the Australian Institute of Health and Wellness.
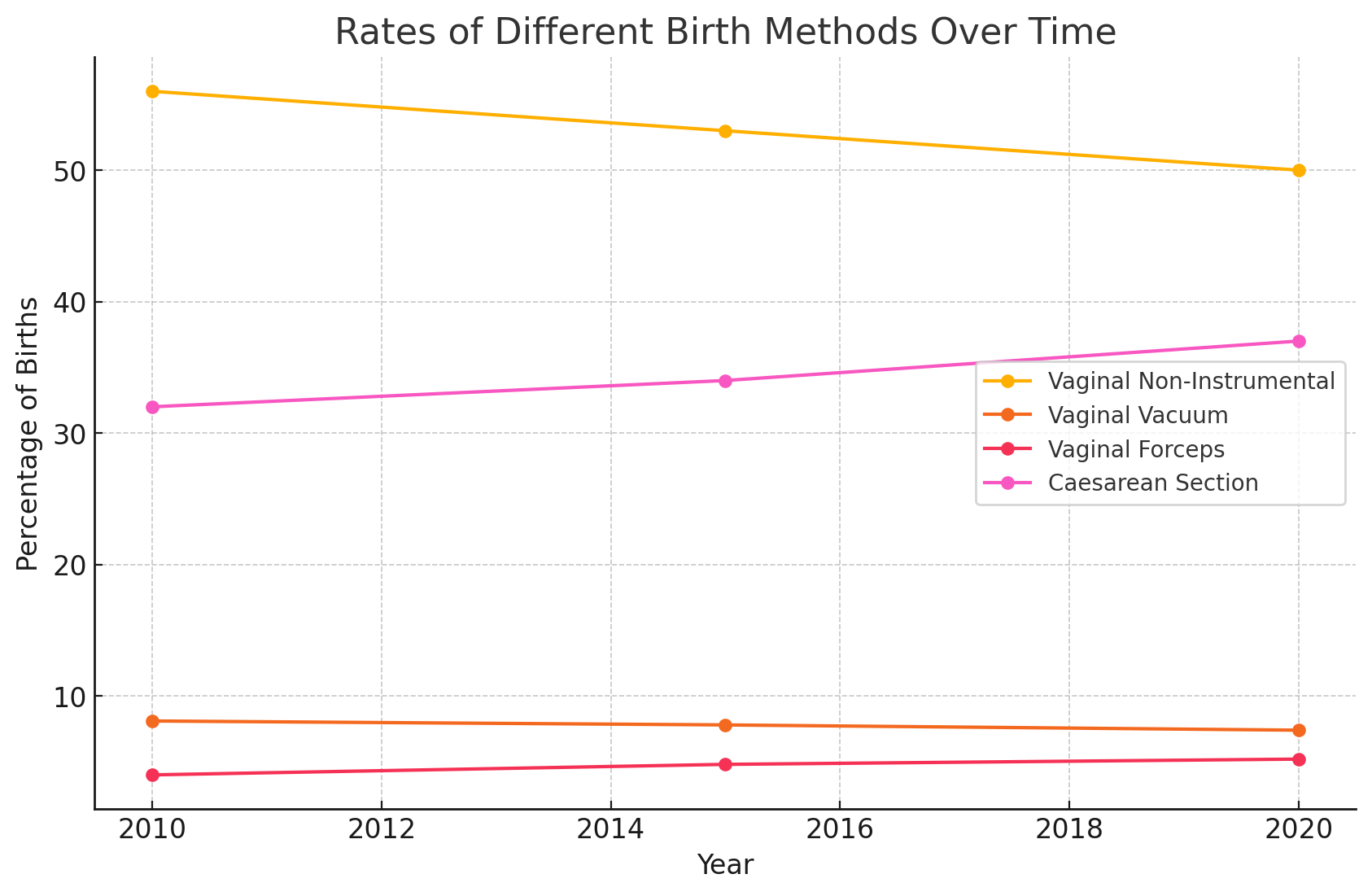
Over time, the proportion of women who had a vaginal non-instrumental birth has decreased, and the proportion of women who had a caesarean section birth has increased. Vaginal birth assisted by vacuum or forceps has remained relatively stable. In 2020 these statistics were:
- 50% of women had a non-instrumental vaginal birth (compared with 56% in 2010).
- 7.4% of women had a vaginal birth assisted by vacuum (compared with 8.1% in 2010).
- 5.2% of women had a vaginal birth assisted by forceps (compared with 4.0% in 2010).
- 37% of women had a caesarean section birth (compared with 32% in 2010).
Oxytocin Use and Neurodevelopmental Outcomes
The point around this is towards stress on the child with the possibility of inducing alteration in oxygen supply to the baby in a critical juncture of life. The birth generally takes a period of time to adjust the baby to the new environment, which is filled with oxygen. From Eastman’s paper: “The fetus exists in a continuous state of cyanosis, a fact that is not only documented by countless blood oxygen studies but is plainly apparent at any caesarean section. The degree of cyanosis is such that it is rarely seen in extrauterine life and, when it does occur, the subject is frantically gasping for breath; in addition, he is usually moribund.” The point being is that the activation of the MORO, ATNR, TLR, and GALANT reflex among others prepare the child over the several hours of a natural vaginal delivery to get ready for the high oxygen world, thus perhaps the sudden exit via the surgical opening without the preparatory phase and primitive reflex activation could be considered unrestrained hyperoxia inducing brain cell tissue damage from oxidative stress and significant inflammation as discussed above.
The fetus prior to birth appears to thrive on the low oxygen pressures normally provided for it. Unfortunately, however, because of certain vagaries of uterine contractility and placental behavior, this meager oxygen supply is sometimes depressed even lower than usual; and this the fetus cannot endure for more than a few minutes. An average uterine contraction lasting, say, a minute and a half, produces temporary fetal anoxia as evidenced by the invariable slowing of the fetal heartbeat. But if this same contraction should last five minutes as sometimes happens, from the injudicious use of oxytocic drugs which are used for induction, then there is a well-known risk that the fetus can die forthwith from anoxia.
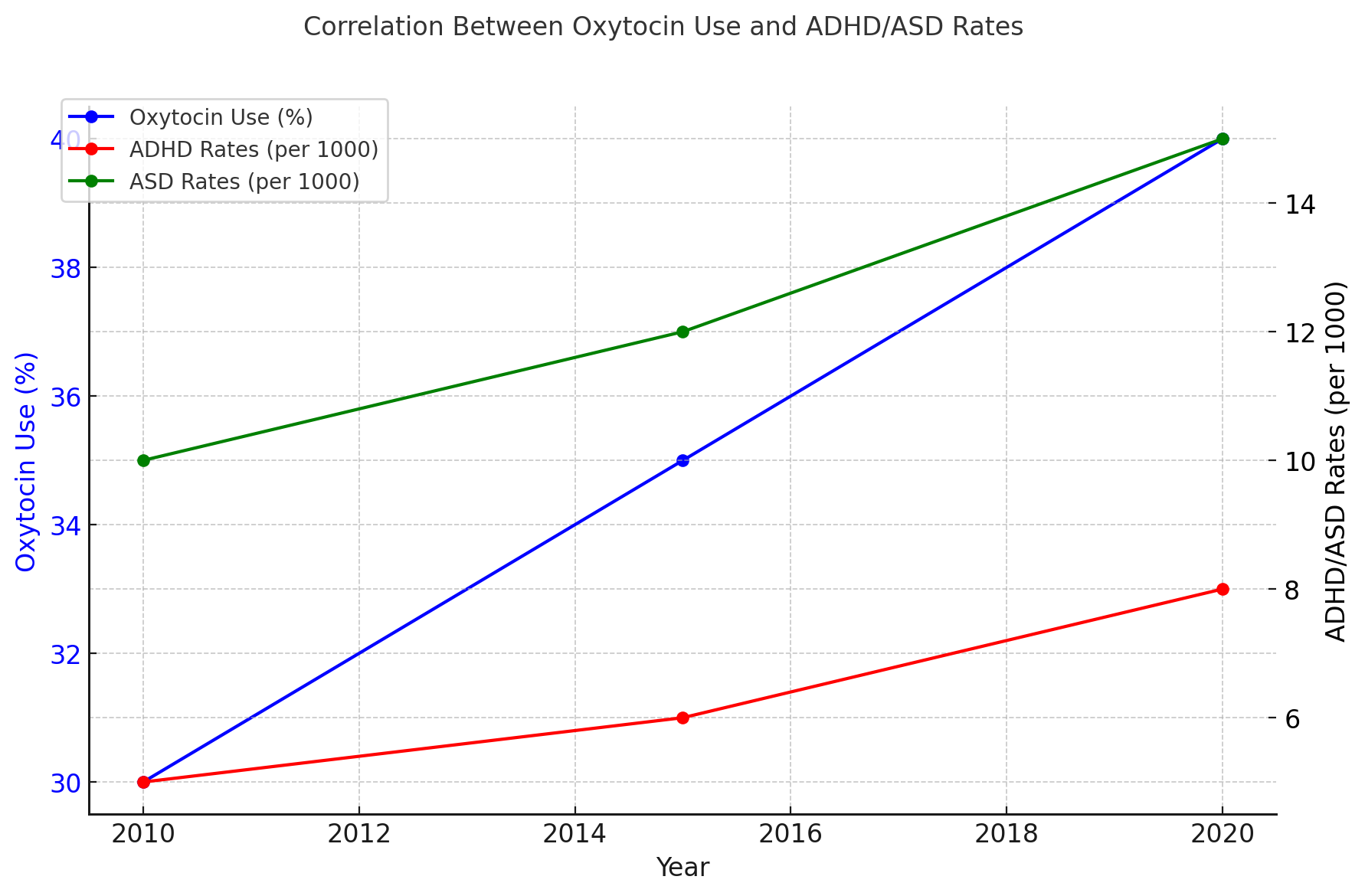
It appears that oxytocin use to induce delivery has increased in recent years with a paper from 2021 on a cohort of Danish and Finnish children showing oxytocin was used in 31% and 46% of the included deliveries in Denmark and Finland, respectively. Interestingly they noted a correlation which has not yet reached causation (only time will tell) between synthetic oxytocin use in birth and ADHD and ASD. Another paper suggested: “Conclusions that perinatal oxytocin increases the risks of neurodevelopmental problems are premature.” There’s a couple of issues to this, first they have concluded this as they determined that observation studies are low quality, regardless of the pool of more than 500,000 children observed for ADHD, and 800,000 for ASD. When digging into the data a bit, we see that there is a 0.45 of a standard deviation decline in cognition on a test of receptive vocabulary (IQ scores) and 0.14 standard deviation units lower on a test of problem-solving ability (z-scores) than the children not exposed to induction with oxytocin. Another study demonstrated increased problem behavior in oxytocin-induced birth, a 2011 study found an increased risk of ADHD with Pitocin induction, while other groups did not, and in the case of oxytocin induction and ASD showed multiple papers with a relative risk above one meaning an increased risk, but the authors decided that the homogeneity between the study groups was low and declined to draw a conclusion suggesting a change in obstetrics rules is required. As the father of an ASD child who was induced with synthetic oxytocin, I do feel a little biased in the opposite direction from the researchers' conclusions. Another group found an increase in ADHD in induced children but managed to explain it all away by families having similar ADHD diagnosis rates. This makes it seem that ADHD is a magic occurrence or that it's simply genetic, which has been stubbornly hard to prove. There simply is no single gene for ADHD or ASD.
Synthetic Oxytocin and Its Effects
However, what if the neurodevelopmental change was more related to where we started, as Eastman spoke about in his 1954 paper. This being that oxytocin can cause anoxia, which at that point was mainly associated with cerebral palsy. He reported experiments on guinea pigs who were asphyxiated at birth and demonstrated cognitive issues as adults. These experiments were designed to simulate the conditions of infants born anoxic. Many of these fetuses showed obvious brain damage and neurological aberrations during the early neonatal period. The subjects lost more defects and were apparently like the normal controls. However, permanent impairment of learning ability was demonstrated. At adulthood, they learned more slowly and forgot more quickly than the controls. The highest brain centers were thus the ones most permanently damaged. This resembles closely the ASD situation.
Perhaps, therefore, it’s the dose and the duration of the exposure to synthetic oxytocin that might make the difference to the developmental outcomes. Meaning that if it's high for longer, perhaps the child becomes more anoxic and creates greater oxidative stress to sensitive neuronal pools? But a lower dose may drive acidification and alter methylation, fibroblast differentiation, and alter connective tissue development in the newborn. What if the anoxic child is reperfused with a high dose of oxygen soon after birth as the Apgar scores were low? This again has a history of neuronal injury.
Recommendations for a Healthy Maternal and Child Environment
Creating a Flourishing Environment

Sadly, there is no definitive answer to any of these questions, which raises the concept of "first do no harm," and if in doubt, don’t. For me, it suggests that as a society, we need to create a mother-flourishing, child-flourishing environment with greater nourishment, less physiological stress, and a lower drive for birth intervention, either elective or inductive. The classic phrase "more research is needed" applies here, but with better questions being asked. The lens needs to shift from "the system is fine, don’t rock it" to "how do we create beautiful, healthy children" and perhaps set systems in place that encourage health, not just a live birth. Something has to be driving the increase in developmental disorders in our kids.
Conclusion
This brings to mind Frederick Douglass' great quote from 1855: “It is easier to build strong children than to repair broken men.” So let's think big together and make the world better for our children and their children.
References
- Nicholson J. Eastman MD, "Mount Everest in Utero," 1954.
- Study on fetal arterial PO2 levels.Perinatal physiologists on hypoxia during birth.
- Study on oxidative stress and free radical conditions in neonates.
- Discussion on maternal stress and primitive reflexes.Cortisol and WNT signaling genetic pathway in "First Principles.
- "Experiment on rat model of folate and B12 deficient mothers.
- Study on defects in folate metabolism during facial development.
- Australian Institute of Health and Wellness statistics.Eastman's paper on fetal cyanosis.Risk of anoxia from oxytocic drug use.
- 2021 paper on oxytocin use in Danish and Finnish children.Correlation between synthetic oxytocin use and ADHD/ASD.
- Study on perinatal oxytocin and neurodevelopmental problems.Frederick Douglass' quote, 1855.

